Pancreatitis: Symptoms, Causes, Types, Diagnosis, Treatment & Expert Care in Agra
Pancreatitis is inflammation of the pancreas, a vital organ behind the stomach that produces digestive enzymes and hormones like insulin. This condition can range from mild and self-resolving to severe and life-threatening. As a leading gastroenterologist, hepatologist, and gastrointestinal surgeon in Agra, Dr. Karan R. Rawat specializes in managing acute and chronic pancreatitis with advanced diagnostics, supportive care, and minimally invasive interventions.
If you’re experiencing severe abdominal pain, nausea, or digestive issues, this SEO-optimized guide covers pancreatitis symptoms, causes, types (acute vs chronic), diagnosis, treatment, and why consulting a specialist like Dr. Rawat at Safe Gastro & Surgery Center is crucial.

What is Pancreatitis?
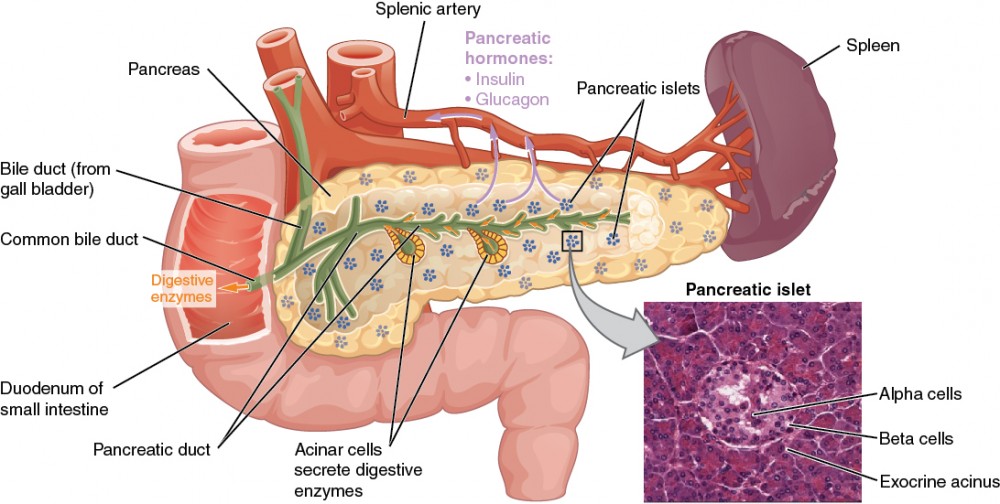
The pancreas aids digestion by releasing enzymes into the small intestine and regulates blood sugar via insulin and glucagon. In pancreatitis, these enzymes activate prematurely inside the pancreas, causing it to digest itself and leading to inflammation, swelling, and potential damage.
Pancreatitis is classified as:
- Acute pancreatitis — Sudden onset, often reversible with prompt treatment.
- Chronic pancreatitis — Long-term, progressive damage with irreversible scarring and loss of function.
Types of Pancreatitis: Acute vs Chronic
- Acute Pancreatitis Sudden inflammation that can be mild (resolves in days) or severe (with complications like organ failure or necrosis). Most cases are linked to gallstones or alcohol.
- Chronic Pancreatitis Ongoing inflammation leading to permanent scarring, fibrosis, and impaired exocrine (digestion) and endocrine (insulin production) functions. Often results from repeated acute episodes, heavy alcohol use, or genetic factors.
Causes of Pancreatitis
The most common causes include:
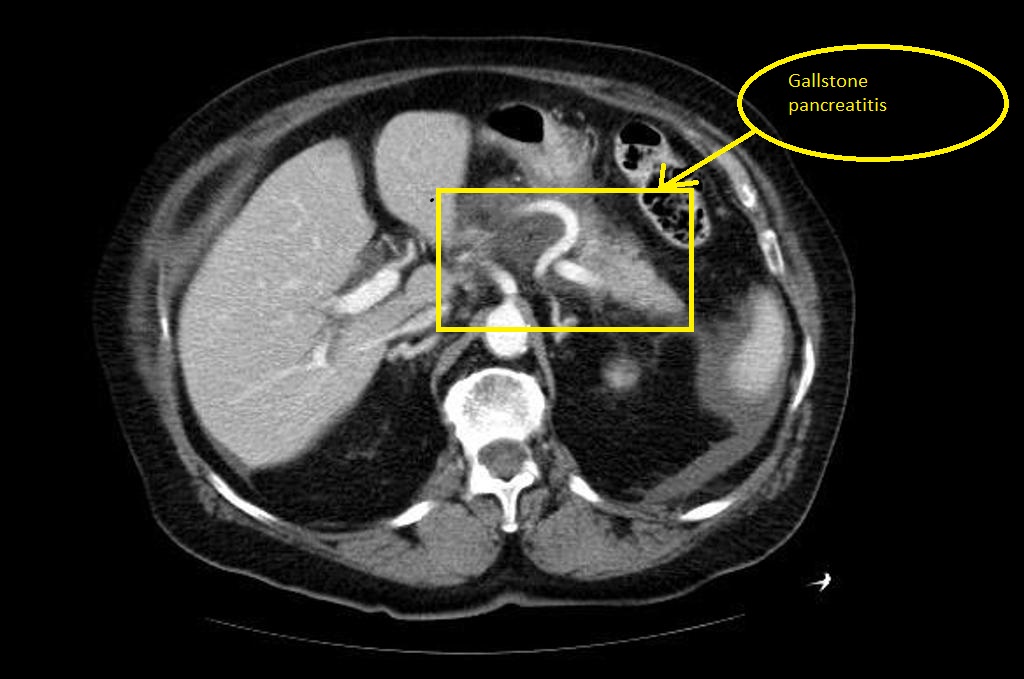
- Gallstones — Block the pancreatic duct, triggering inflammation (especially in acute cases).
- Heavy alcohol consumption or binge drinking — Major cause of both acute and chronic pancreatitis.
- Other factors: High triglycerides, certain medications, smoking, trauma, infections, autoimmune conditions, genetic mutations, or procedures like ERCP.
Symptoms of Pancreatitis
Symptoms vary by type but often include:
Acute Pancreatitis Symptoms:
- Severe, constant upper abdominal pain radiating to the back (worse after eating).
- Nausea and vomiting.
- Fever, rapid heartbeat.
- Abdominal tenderness or swelling.
- Shortness of breath in severe cases.
Chronic Pancreatitis Symptoms:
- Persistent or recurrent upper abdominal pain.
- Unintended weight loss.
- Oily, foul-smelling stools (steatorrhea) due to poor fat absorption.
- Diabetes symptoms (thirst, frequent urination) from insulin deficiency.
- Bloating, indigestion.
Seek immediate medical help for severe pain, persistent vomiting, or fever—these may signal complications like infected necrosis or organ failure.

Diagnosis of Pancreatitis
Diagnosis typically involves:
- Medical history and physical exam.
- Blood tests: Elevated amylase/lipase (≥3x upper limit), liver function, triglycerides.
- Imaging: Ultrasound (for gallstones), CT scan (to assess severity/inflammation), MRI, or endoscopic ultrasound.
- In chronic cases: Fecal elastase (for exocrine function) or glucose tolerance tests.
Early diagnosis prevents complications—guidelines (e.g., 2025 IAP/APA) emphasize supportive care and avoiding unnecessary early imaging.
Treatment for Pancreatitis
Treatment focuses on resting the pancreas, managing symptoms, and addressing causes.
Acute Pancreatitis Treatment:
- Hospital admission for IV fluids, pain relief, and monitoring.
- Fasting initially, then gradual nutrition (oral or tube feeding).
- Treat underlying cause (e.g., ERCP for gallstones, alcohol cessation).
- Antibiotics only for proven infection (per 2025 guidelines).
- In severe/necrotizing cases: Delayed intervention (4+ weeks) with minimally invasive drainage or necrosectomy.
Chronic Pancreatitis Treatment:
- Pain management, enzyme supplements for digestion.
- Insulin for diabetes.
- Lifestyle changes: Stop alcohol/smoking, low-fat diet.
- Endoscopic or surgical procedures for duct issues, pseudocysts, or pain relief.
Most acute cases resolve with supportive care; chronic requires long-term management to prevent progression.

Chronic Pancreatitis – Harvard Health
Why Choose Dr. Karan R. Rawat for Pancreatitis Treatment in Agra?
Searching for the best gastroenterologist in Agra, pancreatitis specialist near me, acute pancreatitis treatment in Agra, or chronic pancreatitis doctor in Agra? Dr. Karan R. Rawat is the trusted expert.
At Safe Gastro & Surgery Center, Church Road, Agra, Dr. Rawat offers:
- Expert diagnosis and management of acute/chronic pancreatitis.
- Advanced endoscopy, ERCP, and minimally invasive procedures.
- Comprehensive care for related issues like gallstones, diabetes, and digestive complications.
- High success rates with patient-focused, evidence-based approach (aligned with latest 2025 guidelines).
With qualifications including MBBS, MS (General Surgery), FMAS, DMAS, FICRS, FIAGES, and recognition as Agra’s leading laparoscopic, laser, and robotic surgeon, Dr. Rawat provides compassionate, effective care.
Conclusion: Don’t Ignore Pancreatitis Symptoms
Pancreatitis can be serious, but timely intervention leads to excellent outcomes—especially in acute cases. Lifestyle changes like avoiding alcohol and managing gallstones prevent recurrence.
If you’re in Agra experiencing abdominal pain, nausea, or suspect pancreatitis, consult Dr. Karan R. Rawat today. Call +91 7398888889 or visit www.surgeoninagra.com to book an appointment.
Protect your pancreas—expert GI care is available right here in Agra!
